Latest Resources
Elizabeth Ripley of the Mat-Su Health Foundation to Be Honored with the 2025 Terrance Keenan Leadership Award
Elizabeth Ripley, President and Chief Executive Officer of the Mat-Su Health Foundation in Alaska, will receive Grantmakers In Health’s 2025 Terrance Keenan Leadership Award.
Jane Perkins of the National Health Law Program to Be Honored with the Andy Hyman Award for Advocacy
Jane Perkins, Litigation Director of the National Health Law Program (NHeLP) in Washington, DC, will receive Grantmakers In Health’s 2025 Andy Hyman Award for Advocacy.
Data Show That The Majority of Adult Medicaid Enrollees are Working
Amid renewed interest in Medicaid work requirements as part of a broader legislative package designed to significantly reduce federal Medicaid spending, KFF has updated its analysis of the work status and demographic characteristics of Medicaid enrollees with the latest data.
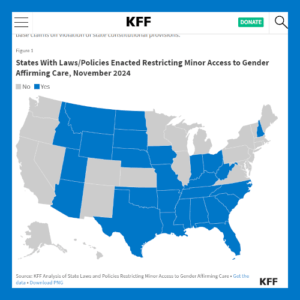
Youth Access to Gender Affirming Care at the Supreme Court: What to Know
Ahead of December 4 arguments in a Supreme Court case (U.S. v. Skrmetti) challenging the constitutionality of Tennessee restrictions for gender affirming care for minors, KFF explores the background of the case and potential rulings.
Biden-Harris Administration Announces $75 Million Investment in Rural Health Care
The Health Resources and Services Administration (HRSA), an agency of the U.S. Department of Health and Human Services (HHS), announced nearly $75 million to support health care services in rural America. Funding will launch new opioid treatment and recovery services in rural communities, strengthen maternal health care in the South, and help rural hospitals stay open.
Health Foundation for Western & Central New York: August 2024
In this report, “How to Maximize Health Insurance Enrollment: Funding Local Marketing and Outreach Innovations by Community-Based Enrollment Agencies”, the Community Service Society of New York analyzed outcomes from a pilot program and the strategies deployed to enroll uninsured individuals who were eligible for affordable coverage.
The Commonwealth Fund: August 2024
The 2024 State Scorecard on Women’s Reproductive Health has been released based on the most recent data to assess how well the health care system is working for women in every U.S. state. It measures performance by 32 different metrics across three areas: health outcomes; health care quality and prevention; and coverage, access, and affordability.
Foundation for Opioid Response Efforts: July 2024
The Opioid Crisis Innovation Challenge marks an expansion of FORE’s Innovation Program, which was launched in 2022 to support projects that combine strategies from diverse fields and engage multidisciplinary teams in tackling some of the most intractable problems associated with the nation’s opioid-related addiction and poisoning crisis.
Connect With Funder Peers on Access
Interested in exchanging strategies, information, and questions with your funder peers? Sign up for GIH E-Forums.