Cat Hulburt, Senior Director, U.S. Programs, Americares
Ashley Edwards, Director, U.S. Programs, Americares
Madison Bates, Associate, U.S. Programs, Americares
Each year, more than two million low-income, uninsured, and underinsured people in the United States rely on approximately 1,400 nonprofit free and charitable clinics and charitable pharmacies for essential health care (Darnell et al. 2022). These clinics use a volunteer/staff model to provide a wide range of health services including medical, dental, pharmacy, vision, and behavioral health services. Many clinics also address social needs, such as connecting patients to housing, food assistance, or employment assistance programs.
Despite all the programs and services free and charitable clinics provide, there was no national apparatus in place to systematically collect and report data to measure the clinics’ quality of care or to identify health inequities prior to 2017. Existing publications regarding free and charitable clinics focused on small patient populations or one-clinic case studies. With no federal reporting requirements unlike Federally Qualified Health Centers, there had been no benchmark data available to compare performance. This made it challenging to evaluate whether patients served by free clinics were receiving the care they needed when they needed it, and whether their health was in fact improving. Further, it was complicated to determine if clinics were providing equitable access to care and quality treatment, regardless of demographics such as race or gender.
Roadmap to Health Equity
In 2017, the Roadmap to Health Equity initiative was founded by Americares and the National Association of Free and Charitable Clinics, with support from Loyola University Chicago and a consortium of stakeholders including state-level free and charitable clinic associations and individual clinics from across the country. With the goal of reducing inequity and delivering high quality care in clinics nationwide, Roadmap has created the first national data repository for free and charitable clinics. Currently, the program has more than 75 clinic partners nationwide and has been collecting data since 2020. While the data repository is a key facet of the program, Roadmap also offers technical assistance, quality improvement programming, grants, peer learning calls, and other resources for clinic partners.
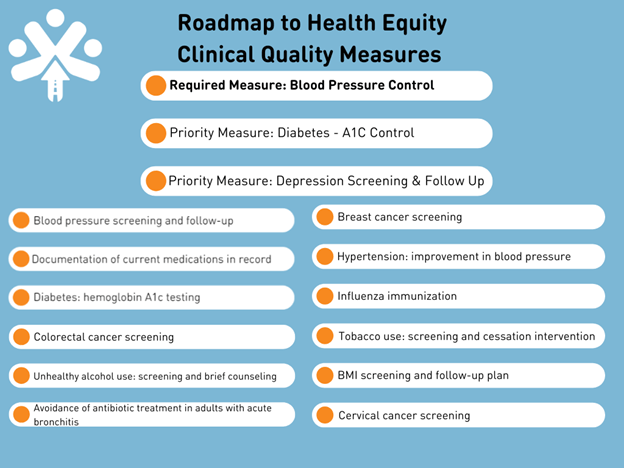
Annual data submission happens each year between January and March, with clinics submitting data on up to 15 clinical quality measures, as illustrated in the chart below:
Data
As of 2024, over 60,000 patients were represented by the Roadmap dataset, from 61 clinics and 26 states. This data helps clinics convey their work and impact to funders and volunteers, increasing visibility and recognition. Some findings from the 2023 annual data are below:
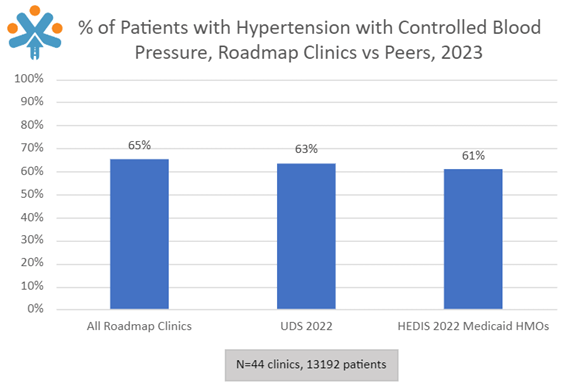
- 65.22 percent of patients 18-85 years of age who had a diagnosis of hypertension overlapping the measurement period had their blood pressure adequately controlled (<140/90mmHg);
- 51.84 percent of patients over 12 years old were screened for depression and, if positive, adequately connected to follow up care;
- 25.47 percent of patients 18-75 years of age with diabetes had poorly controlled hemoglobin (A1c > 9.0%) during the measurement period ; and
- 66.36 percent of eligible female patients received breast cancer screening during the measurement period.
In addition to this clinical quality data, Roadmap collects data on sociodemographic characteristics, including race, ethnicity, age, language barrier, and sex at birth. Clinics can review stratified, clinic-level data and compare it to other similar clinics and external benchmarks (example below).
To take full advantage of Roadmap, clinics receive a comprehensive suite of supports, including one-on-one calls with Roadmap staff and partners, meetings with a data consultant, recorded videos, how-to guides, live trainings, and more.
Acting on the Data
“BEING ABLE TO EXPAND OUR ANALYTICS CAPABILITY HAS MADE US MORE CERTAIN ABOUT OUR CARE. IT HAS ALLOWED US TO ZERO IN ON A SUBSET OF PATIENTS THAT NEED MORE SUPPORT SO THAT WE COULD TICK THOSE MEASURES UP IN A MEANINGFUL WAY.”
After receiving their disaggregated data and the full Roadmap comparison data, clinics are encouraged to identify and act upon disparities found on each measure. Several Roadmap programs support clinics in this endeavor, with dozens of additional online resources available on the Roadmap website. One such program was the Addressing Disparities in Health Outcomes program, which sponsored nine Roadmap clinics as they participated in rigorous quality improvement coaching to address identified disparities in their patient population. Clinics identified disparities in their A1C care, depression screening, and blood pressure control. Working with an Institute for Healthcare Improvement consultant, clinics ran Plan-Do-Study-Act cycles at various levels of their clinic operations and were able to see improvements.
Further programming to support quality improvement continues within Roadmap. In spring 2024, Roadmap launched a Mental Health Peer Learning Series to support clinics in implementing depression screening among patients, with additional programs planned for the future.
Future Directions and Clinic Experience
Roadmap continues to increase partnerships with state associations, including a flagship partnership with the South Carolina Free Clinic Association that will bring all South Carolina free clinics to Roadmap by 2025, and expand the supports available to participating clinics. Roadmap clinics now routinely utilize their data to make more informed decisions to address inequities and improve patient outcomes. Thanks to Roadmap, they can now back up their impact stories with clinical quality data to demonstrate value and highlight key areas where improvements can be targeted.
Learn more about Roadmap to Health Equity by visiting healthroadmap.org.
“FOR ME IT’S THE TRUE BELIEF THAT THIS IS IMPORTANT. I THINK THAT FOR THOSE WHO’VE BEEN IN THE FREE CLINIC SECTOR FOR A LITTLE BIT OF TIME, THIS IS THE NEXT FRONTIER TO LEGITIMIZE WHAT WE DO.”
References
Darnell, Julie S., Michael Perry, Nicole Lamoureux, and Edith Lee. “Don’t let perfect be the enemy of good: a proof of concept for a custom national data repository of quality measures for free and charitable clinics.” Health Equity 6:1 (2022): 708–716. doi:10.1089/heq.2022.0078.

