Andrea Palmer, Program Officer, Pritzker Children’s Initiative
Jacque Caglia, Director of Learning, Communications and U.S. Programs, Merck for Mothers
Wilna Paulemon, Associate Director of U.S. Programs, Merck for Mothers
Raquel Mazon and Wendy McWeeny, Co-Directors, Community Health Acceleration Partners
Alexandra Geertz and Leah Nakon, Founding Partner and Advisor, Afton Bloom
As state policymakers began extending continuous eligibility for postpartum Medicaid coverage from the 60 days following birth to the 12 months following birth in 2022, a small workgroup of funders connected to explore what philanthropy’s role could be in strengthening maternal health outcomes and how we might support effective implementation of the extension. Since Medicaid covers about 41 percent of births nationally, with higher rates in Southern states (Centers for Medicare & Medicaid Services 2024), this policy decision represented a unique opportunity to improve perinatal health outcomes. We were particularly concerned with barriers to states implementing coverage in ways that address ongoing inequities in postpartum mortality and morbidity that led to nearly 700 people dying in 2023 due to pregnancy related complications in the U.S., including homicide, suicide, drug overdose, and hemorrhage.
The workgroup, which included Pritzker Children’s Initiative, Merck for Mothers, and Community Health Acceleration Partnership, formed in August 2023 to identify timely opportunities to ensure state Medicaid coverage extensions effectively addressed the root causes of postpartum morbidity and mortality.
Ultimately, we were committed to the goal of ensuring culturally competent, community-driven approaches to policy implementation. Over the course of the year the group worked to:
- Understand the current state of postpartum Medicaid coverage,
- Identify barriers to uptake and use of coverage,
- Assess the current state of evidence concerning standards of care beyond the six weeks following birth (also known as the “fourth trimester”), and
- Learn how funders could help improve postpartum outcomes and ensure the effectiveness of the coverage extensions by mobilizing funding and attention.
Identifying the Key Issues
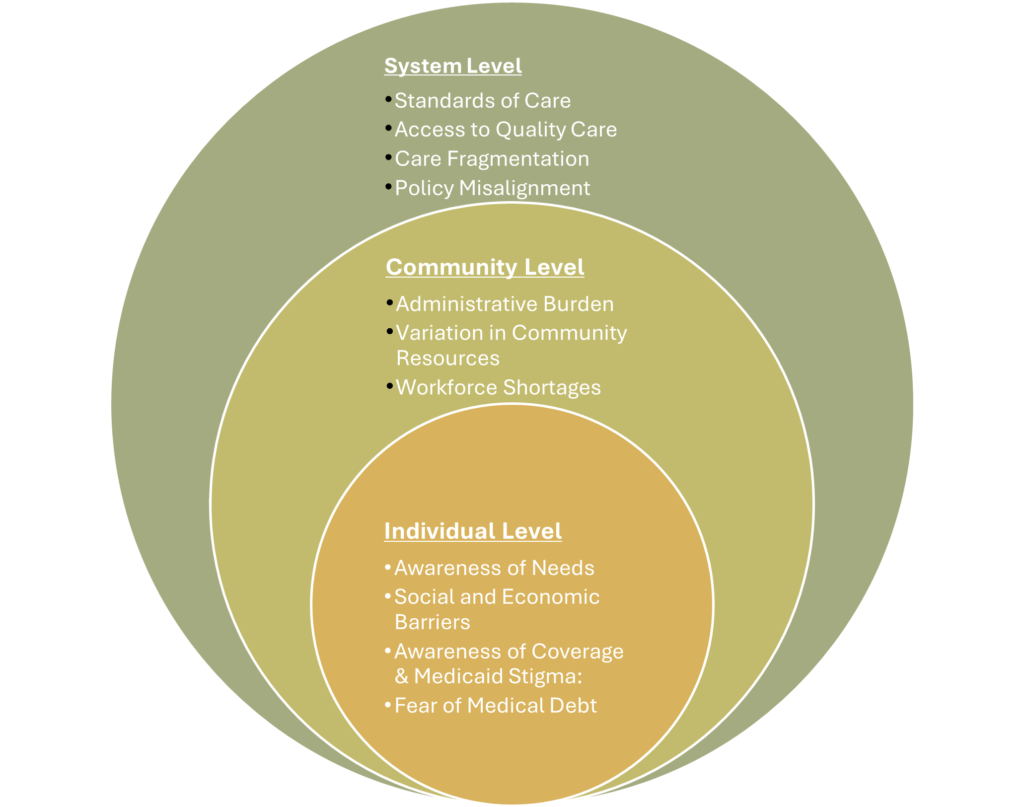
During our first gathering, we decided that the first step was to listen to leaders across sectors to assess the state of Medicaid coverage and how coverage shapes access to care. All three funders have extensive experience working with state leaders and peers and were acutely aware of the need to develop a nuanced understanding of the barriers and opportunities to effective policy implementation. Over the course of three months, Afton Bloom conducted interviews on behalf of the workgroup with policymakers, researchers, and advocates across the nation. These conversations revealed a deep fragmentation of care and little coordination of mental, physical, social, and economic services during postpartum. Interviews also surfaced the lack of an accepted standard of postpartum care that addresses comprehensive psycho-social needs, including, but not limited to substance-use disorder and intimate partner violence. The current clinical standard of care for the postpartum period is limited to the fourth trimester, or the 12-week period following birth. Federal policy, such as the Family and Medical Leave Act and clinical guidelines from the American College of Obstetrics and Gynecology mirror this timeline. However, the clinical standards of care are not based on quantitative or qualitative evidence about postpartum needs. This lack of clinical evidence is compounded by a lack of shared cultural norms around postpartum recovery. Despite upticks in clinical and community-based research about postpartum care and quality standards, there is no widespread consensus about the ideal arc of postpartum recovery and the infrastructure needed to advance such care.
Understanding What is Working
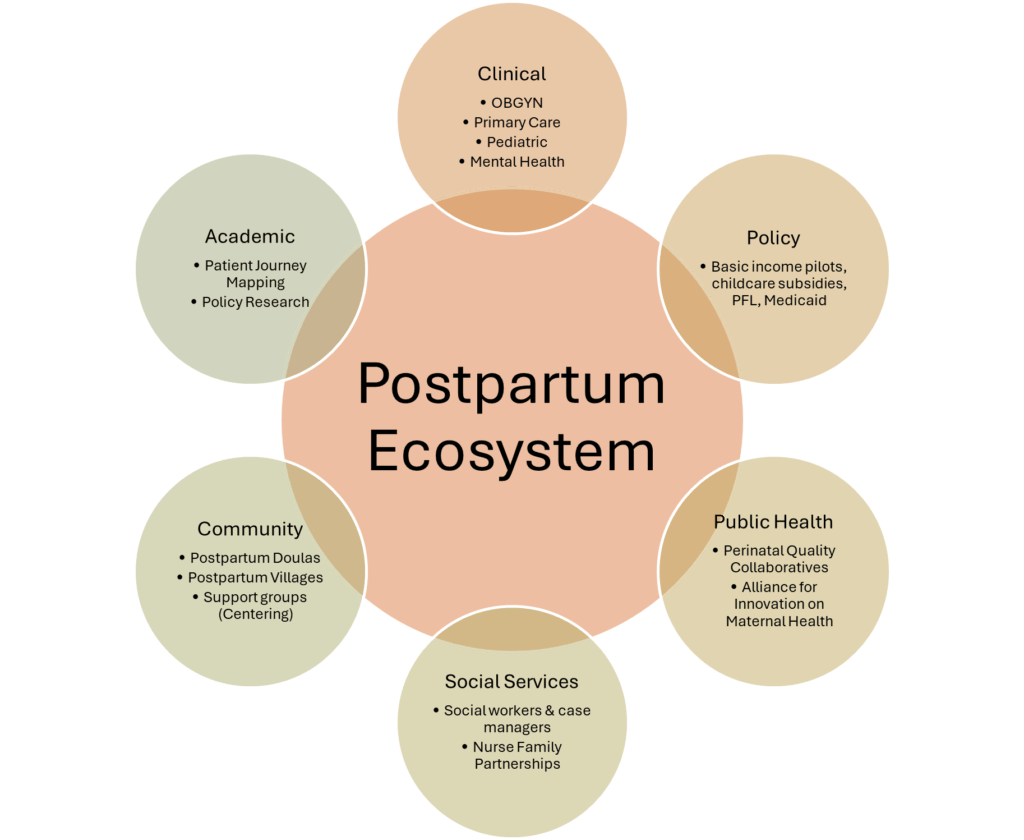
In addition to understanding the key barriers, we wanted to better understand the variety of responses across sectors to addressing key challenges and barriers. The landscape scan surfaced dozens of inspiring efforts designed to address postpartum care needs including work to a) improve the research and practice related to postpartum care standards; b) recover midwifery-inspired dyadic models of care; c) address the clinical and community care professional shortages; and d) educate potential and current Medicaid enrollees and providers about coverage and benefits.
Our research revealed that the most comprehensive work needed is to research and develop a comprehensive standard of care that addressed clinical needs and systems level needs. A diverse array of clinical and community-based care teams are looking at ways to recover the midwifery-based model of dyadic care. These models are seeking to build or connect existing health care infrastructure and community-based programming to provide clinical and mental health services to parents and infants. Other teams are trying to support the clinical and social care providers that serve infants and families during the postnatal and postpartum period. There is a dire shortage and increasing levels of burnout of providers including midwives, primary care practitioners, and mental health practitioners. The workforce tasked with providing support during the postpartum period is uncoordinated and often undercompensated. Finally, there are some efforts underway to ensure individuals and clinicians understand what Medicaid covers beyond contraceptive care.
Connecting the Dots
Despite the number of existing and emerging efforts to address care gaps during the “postpartum cliff”, all interviewees noted that there are limited efforts to coordinate efforts across sectors at the local, state, and national levels. During pregnancy and postpartum an individual might see and provide their health and socioeconomic data to over a dozen care professionals including OBGYNs, family medicine practitioners, pediatricians, midwives, mental health professionals, home visitors, lactation consultants, doulas, social workers/case managers, and/or community health workers. This is a critical gap because, as one physician noted, fixing postpartum is not just about creating clinical guidelines in a silo.
“Postpartum care is about the entire system, not just the clinical environment, but economic stability, mental health, paid family leave, childcare. We haven’t paid attention to it as a system. If we screen patients or have standards and no services to refer to, it feels like malpractice.”
Funders have an opportunity to address this critical gap by creating space and connections that contribute to developing a comprehensive standard of care, supporting ongoing efforts, and ensuring that there is increased attention to the importance of postpartum care and access to Medicaid coverage.
For example, at the state level, the California Health Care Foundation, Packard Foundation, and Merck for Mothers, are supporting the California Department of Health Care Services’ work to develop the Birthing Care Pathway, a model covering the care journey from conception to postpartum for Medi-Cal members. These funders are collaboratively providing support to ensure equitable community engagement in the design and implementation of the birthing care pathway.
Funders continue to play a significant role in supporting organizations and researchers that are working on developing and evaluating models of comprehensive care at the local, state, and national levels. Ongoing funding allows community-based organizations to continue providing person-centered models while integrating new approaches. One innovative effort to provide funding to organizations and projects led by and serving BIPOC communities is the Maternal Mental Health Equity Fund, supported by Perigee Fund, W.K. Kellogg Foundation, Community Health Acceleration Partnership (CHAP), Maritz Family Foundation, and Roots & Wings Foundation, among others. The pooled fund is also providing three years of support for select organizations to participate in a national learning community.
Philanthropic funding has enhanced reproductive health education efforts across the public and nonprofit sectors. National funders like the Commonwealth Fund produced reports to increase national awareness of postpartum care needs and service gaps. Other funders supported educational and awareness campaigns such as the 4th Trimester Project, which developed tools to help individuals, caregivers, and providers recognize and seek postpartum care.
Responding Respectfully
After a year of listening and sharing our findings with peer funders informally and formally at Funders for Birth Justice and Equity and Funders for Maternal Mental Health, we saw a critical opportunity to move beyond raising awareness to supporting efforts to connect and advance the state of care. Each of the workgroup members brought unique vantage points to the work of addressing the structural gaps in postpartum including global, federal, state public health and health policy.
Our diverse career experiences in the field led us to begin with humility. We wanted to honor the supporting role that philanthropy plays in addressing the myriads of social, economic, and medical issues that have contributed to the treacherous nature of the “postpartum cliff”. At the same time, we wanted to center our responsibility to leverage our resources in the most effective way. In response to the widespread feedback about the lack of coordination between sectors, the workgroup decided to collaboratively open an RFP for organizations to catalog and connect analogous efforts in the postpartum space to create a centralized hub of resources that inform the development of comprehensive postpartum standards of care. Through centralizing resources, this receptacle will enable researchers, policy makers, healthcare providers, public and private partners and others to access the full scope of work that is happening in the postpartum Medicaid coverage space to create coordination and collaboration within and across sectors.
We are excited about the number of organizations that are interested and well situated to do this work and are eagerly anticipating working with the finalist to continue advancing the state of postpartum care in ways that build bridges and infrastructure to address the postpartum cliff.
References
Centers for Medicare & Medicaid Services. 2024 Medicaid & Chip Beneficiaries at a Glance: Maternal Health. Washington, DC: May 2024.

