Riisa R. Rawlins, Chief Executive Officer, Community Health Commission of Missouri
Reimagining Health Philanthropy Through Community-Led Decision-Making
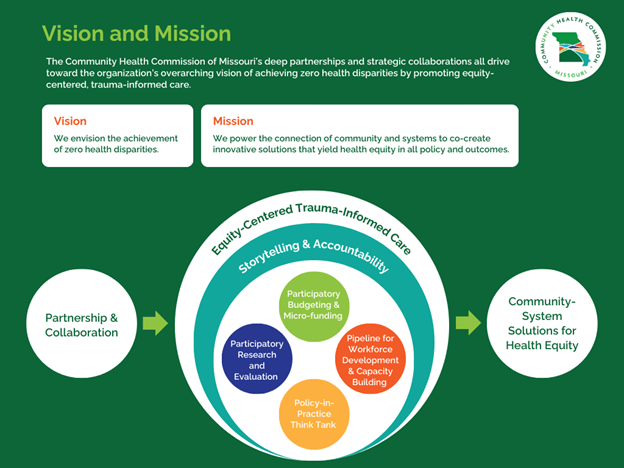
Who is best positioned to determine how health funding should be allocated? At the Community Health Commission of Missouri (CHCM), we believe the answer is clear: the people most affected by health disparities.
Traditional grantmaking models often prioritize funder expertise over the lived experiences of the communities they aim to serve. This disconnect can force community organizations to adjust their work to fit funder-defined criteria rather than investing in what they know works best. Complex application and reporting processes can further exclude organizations that are already creating meaningful impact with limited resources.
Participatory budgeting (PB) offers a proven alternative—one that enhances transparency, trust, and community-led impact by shifting decision-making power to those closest to the issues. PB engages communities in every step of the funding process, from defining priorities to allocating resources, ensuring that investments reflect local needs and lived experiences.
At CHCM, we have embraced this model as a core strategy for achieving zero health disparities. Our Seniors Community Revitalization & Development Fund pilot provided a successful proof of concept, building on lessons from ReCAST STL, a regional participatory grantmaking initiative, and strategic philanthropic partnerships with the Deaconess Foundation.
As funders seek more effective, accountable, and high-impact funding strategies in an evolving socio-political environment, participatory budgeting offers a scalable, results-driven approach to investing in community well-being.
Why Participatory Budgeting? A Smarter, More Accountable Model for Health Funding
As nonprofits and funders rethink their relationships and explore innovative, sustainable funding models, participatory budgeting stands out as an approach that ensures funding reaches where it is needed most.
Key Advantages of Participatory Budgeting:
- Aligns funding with real needs, not assumptions—Local leaders and residents identify the most pressing priorities.
- Strengthens trust and accountability—Community members help shape investments, leading to sustainable, long-term partnerships.
- Maximizes philanthropic impact—Resources are allocated more efficiently, ensuring greater social impact.
- Encourages broad-based collaboration—Fosters strong partnerships between residents, service providers, and funders.
By embedding PB into philanthropy, funders can create a more transparent, community-responsive funding ecosystem that aligns investments with measurable community impact.
Piloting the Model: The Seniors Fund as a Proof of Concept
The Seniors Fund is a case study in effective community-intermediary-philanthropic partnership. As a public health intermediary, CHCM is committed to ensuring every Missourian has access to equitable health care services and support. Our theory of change centers on community-systems partnerships through four key pillars:
- Community-based participatory research and evaluation
- Collaborative policy-in-practice think tanks
- Comprehensive workforce pipelines
- Community-led participatory budgeting and micro-funding
The Seniors Fund pilot allowed us to test and refine the PB model while leveraging a longstanding partnership with the Deaconess Foundation, a regional leader in trust-based philanthropy.
How the Model Worked:
- Listening Sessions: Older adults, caregivers, and community members identified and prioritized funding areas.
- Advisory Board Formation: Older adults and service providers were trained on participatory budgeting and the grantmaking process.
- Collaborative RFP Development: The advisory board created and evaluated applications based on community-defined priorities.
Key Funding Priorities Identified:
- Safety & Accessibility: Home modifications, repairs, and energy assistance to support aging in place.
- Health Navigation: Dementia care support, prescription assistance, and education programs.
- Transportation: Reliable, accessible rides to medical appointments and community events.
Measurable Impact of the PB Model
The Seniors Fund pilot yielded tangible, community-led impact:
- 77+ homes repaired, improving accessibility and safety for seniors.
- 5,520 transportation rides provided, reducing isolation and improving healthcare access.
- Expansion of dementia navigation services, reducing waitlists and enhancing family support.
- Strengthened community engagement and trust, as local leaders played a direct role in funding decisions.
As a nonprofit public health intermediary, CHCM bridges philanthropy, health systems, and communities to ensure equitable resource allocation. PB strengthens this model by keeping funding grounded in community priorities while leveraging the expertise of philanthropy and public health systems.
Bridging the Gap: Participatory Budgeting as a Sustainable Strategy Amidst Shifting Funding Priorities
Programs focused on racial equity, disability justice, immigrant health, and gender-based disparities are facing funding losses due to shifts in public and private funding priorities. While these changes present challenges, they also offer funders an opportunity to rethink how resources are distributed.
Participatory budgeting offers a sustainable solution to ensure continued investment in communities that have historically faced systemic health inequities:
- PB builds resilient funding streams—Embedding community-led decisionmaking into grantmaking ensures sustained investment in equity-centered work, even as traditional funding sources fluctuate.
- PB focuses on practical impact, not ideology—Grounded in efficiency, accountability, and data-driven decisionmaking, PB provides funders with a nonpartisan, results-oriented framework that withstands political and economic shifts.
- PB directs resources to those facing the greatest need—Ensuring communities continue to receive critical support, even when funding priorities change.
By institutionalizing PB, funders can safeguard investments in health equity from political and economic volatility while strengthening trust, transparency, and community impact.
Scaling the Model: Lessons from ReCAST STL
CHCM’s experience with PB builds on its participation in ReCAST STL (Resiliency in Communities After Stress and Trauma), a regional initiative that applied participatory decisionmaking to invest in trauma recovery, behavioral health, and economic opportunity.
Key Lessons from ReCAST STL for Expanding PB in Health Funding:
- PB is adaptable and scalable—It can be applied across public health, social services, and economic development.
- Cross-sector collaboration is key—Engaging funders, government agencies, and community leaders strengthens impact.
- A structured, transparent process leads to better outcomes—Clear guidelines and ongoing engagement maximize participation and effectiveness.
ReCAST STL demonstrated that when communities have a voice in funding decisions, health outcomes improve. CHCM is now expanding PB into broader health equity initiatives through its threefold partnership model of community, intermediaries, and philanthropy.
A Call to Action for Funders
Participatory budgeting is not just an experiment—it’s a tested, results-oriented model that maximizes the effectiveness of health funding.
Funders have an opportunity to lead by embedding PB into grantmaking structures, prioritizing transparency and accountability.
- PB creates a funding structure that is resilient and adaptable, ensuring investments continue to reach those who need them most.
- Scaling PB is the next step—CHCM invites partners to collaborate in expanding Participatory Budgeting to create a stronger, more equitable health funding ecosystem.
By embracing PB, we can strengthen trust, maximize impact, and build a funding model that works for everyone—especially those historically left out of traditional grantmaking.
Closing Thought
The future of health philanthropy must be community-led, data-informed, and equity-driven. Participatory Budgeting offers a clear, actionable path forward—one where the people closest to the challenges are also the architects of the solutions. Now is the time to invest in community power and scale a model that works.
References
Schugurensky, Daniel and Laurie Mook. “Participatory budgeting and local developments: Impacts, challenges, and prospects.” Local Development & Society. Volume 5, Issue 3 (August 16, 2024): 433-445.

